Coxa Saltans, also known as the “Snapping Hip Syndrome”, is a clinical condition characterized by an audible or palpable snapping sensation that is heard or felt with hip movement. The snapping hip has multiple etiologies and is classified based on the anatomical structure that is the source of the sensation. Typically, this condition is patients in their teens to early 20’s. It is characterized by an audible snap or pop that occurs with flexion and extension of the hip. Although it normally felt during exercise, it can occur during activities of daily living. Patients report the audible sound is felt about the lateral hip region with flexion, extension and abduction. The pain may radiate down to the knee. Several causes of this clinical entity have been implicated and classified as to the anatomic location.
The etiology was classified as extra articular or intra articular. Recently with further investigation into the causes the classification has been changed to External Snapping Hip and Internal Snapping Hip.
Intra articular etiology should also be mentioned. This includes labral tears, loose bodies, osteochondral lesions, hip subluxation and synovial chondromatosis.
External Snapping Hip
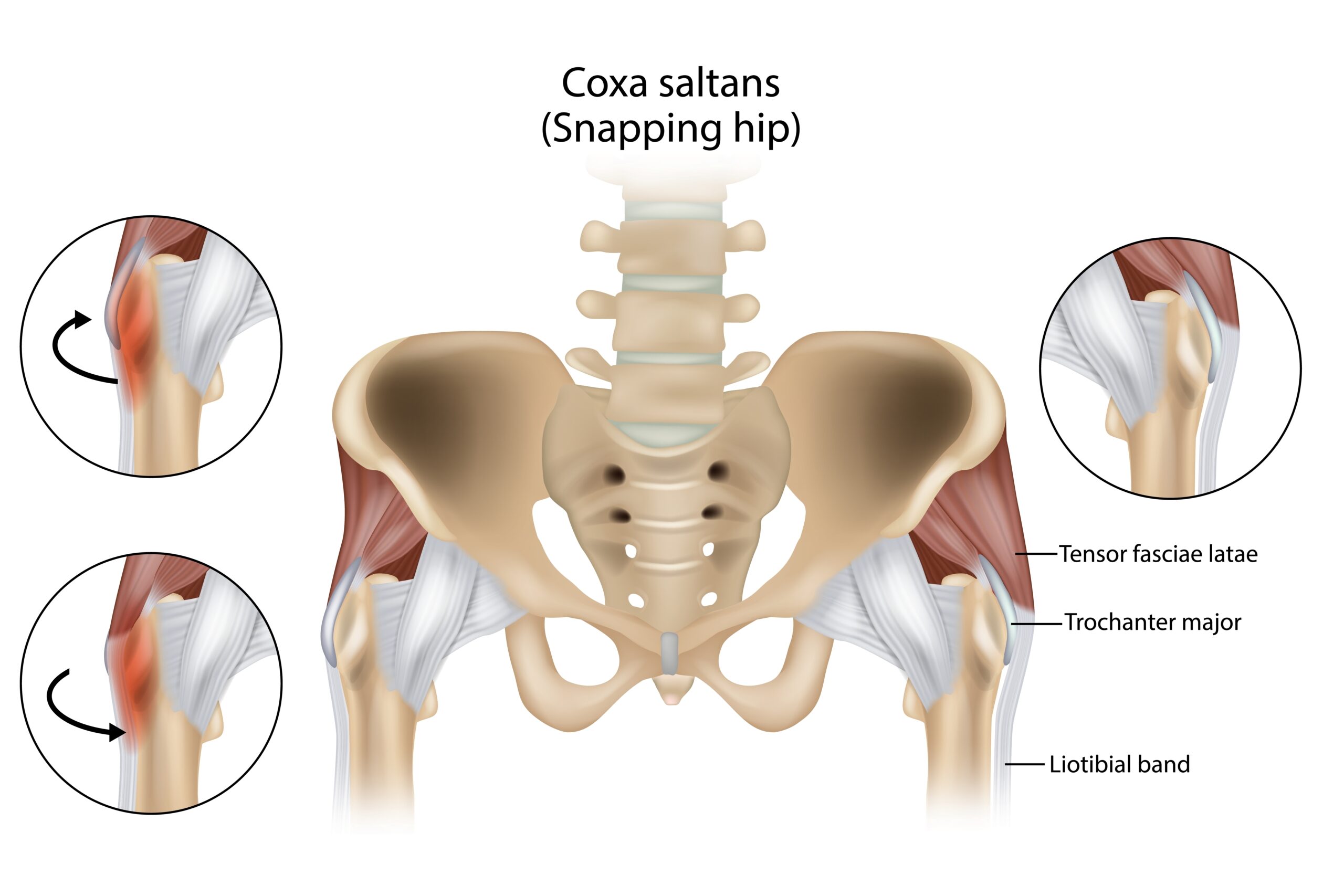
The External Snapping Hip is most likely caused by the iliotibial band moving over the greater trochanter of the femoral head during hip motion. These movements include hip flexion, extension, internal and external rotation.
Other causes of external snapping hip include:
- Hamstring tendon rolling over the ischial tuberosity
- Fascia lata or gluteus maximus rolling over the greater trochanter
- Psoas tendon rolling over the iliac muscle fibers
- Combination of the above such as iliotibial band and gluteus maximus snapping over the greater trochanter during the same motion of the hip
Internal Snapping Hip
The Internal snapping hip commonly occurs as the iliopsoas tendon travels and snaps while traveling over bony prominences such as the anterior femoral head or the iliopectinal eminence. Also, this snapping can mimic intra articular pathology of the hip. In greater than 50% of internal hip cases, intra articular hip pathology is found.
Other Pathologic Conditions Causing Similar Symptoms
- Synovitis
- Iliotibial Band Syndrome
- Articular loose bodies
- Hip Tendonitis
- Avascular Necrosis
- Labral Tears
- Bursitis, Greater Trochanteric or Iliopsoas
Epidemiology
Approximately 5-10% of the population is affected by coxa saltans. The majority of these cases experience painless snapping.
The prevalence is greater in women than men. Most, if not all, of these cases involve repetitive hip motions. In sporting activities, ballet dancers, weightlifting, soccer players and runners report snapping to be a common occurrence.
In ballet dancers, 90% report snapping and 50% have snapping bilateral. Ballet movement that causes this syndrome include external hip rotation and abduction over 90 degrees.
Snapping hip is commonly an overuse problem. It can also be precipitated by trauma and surgery. Following total hip arthroplasty, the smaller femoral neck angle has been linked to this problem. Iliotibial band tightness, shorter tendon lengths, muscle tightness may all contribute to coxa saltans.
Pathophysiology
Internal snapping hip is most commonly caused by the iliopsoas tendon snapping over bony areas. Patients report the classic symptoms of pain with an audible snap and point to the area of the anterolateral hip or groin.
External snapping hip is caused by the iliotibial band snapping over the greater trochanter of the femoral head during hip movements. Patients will complain of snapping and pain over the lateral hip.
Evaluation
History and physical exam can often aid pinpoint the anatomic region of the snapping. The patient can often precipitate the snap with hip movement. However, other hip pathologies should be ruled out.
It should be noted, the majority of intra articular pathologies have a different presentation than coxa saltans. The patients describe a click rather than a snap. These patients often have significant pain. They may also state that the hip catches or gives away. They often have a history of trauma, hip dislocation or hip dysplasia in past years.
Plain X-rays are of little help to confirm the diagnosis however they are often the first test ordered to rule out anatomic variations, developmental abnormalities or other hip pathologies.
Lidocaine anesthetic injections in the affected area can help distinguish between internal and external etiologies.
MRI may confirm a thickened iliotibial band or thickened edge of the gluteus maximus.
Dynamic ultrasound can be used to visually examine the site of the snap. Ultrasound can also reveal tendonitis, iliopsoas bursitis or muscle tearing.
MRI arthrography is the preferred method of diagnosis because it can also detect intra- articular pathology which commonly accompanies internal snapping.
Treatment
If pain is not present, treatment is not warranted. When pain is present during or after snapping, conservative treatment is usually initiated. This consists of rest, stretching, oral anti-inflammatory medications, physical therapy, activity modification and steroid injections. Multiple steroid injections are typically needed.
If these measures fail, surgery is considered. For external snapping, loosening of the iliotibial band is accomplished by open surgery or arthroscopic technique. If the iliotibial band is loosened or completely released, weakness in hip abduction may result. Weakness is also a common side effect of this procedure.
For internal snapping hip syndrome, open or arthroscopic procedures are used to lengthen or release the iliopsoas tendon. The most common side effect of this surgery is hip flexor weakness which may occur with excessive release or damage to other tissues.
Corrective surgeries for either internal or exterior snapping hip have potential side effects than previously stated. These include infection, muscle damage or atrophy nerve damage or continued symptoms. Ossification can also occur in the tendon.
Platelet Rich Plasma
Platelet Rich Plasma is an autologous blood concentrate rich in cytokines, growth factors and bio-active proteins. Platelet Rich Plasma has been used in all fields of medicine, dentistry and veterinary to promote repair and to rejuvenate damaged or aging tissues. In applications where steroids have been used, platelet rich plasma has been found to be equally efficacious and far superior in extended time periods. Since Coxa Saltans is a problem of tendons, and steroids cannot be injected into tendons, platelet rich plasma appears to be a superior treatment choice.
Studies
Br Med Bull 2021 Sep 10;139(1):86-99 PMID 34405857
Introduction: Greater trochanter pain syndrome is characterized by a persistent and debilitating pain around the greater trochanter. GTPS can be caused by a combination of gluteus medius or minimus tendinopathy, snapping hip, or trochanteric bursitis.
Areas of agreement: Platelet rich plasma and corticosteroids are useful options to manage symptoms of GTPS.
Points investigated: A systemic review and meta-analysis comparing PRP vs CCS was conducted.
Conclusion: PRP injections are more effective than CCS
Arthroscopy 2020 Mar;36(3):875-888 PMID 31882270
Purpose: To perform a systematic review of the outcomes of platelet rich plasma injections as an in-office procedure versus surgical treatment for recalcitrant greater trochanteric pain syndrome.
Conclusion: Both PRP and surgical intervention for the treatment of recalcitrant GTPS showed statistically and clinically significant improvements. PRP injections provides an effective and safe alternative.
J Hip Preserv Surg. 2018 Aug;5(3): 209-219. PMID 30393547
Purpose: This review aims to determine whether platelet rich plasma has any role in improving clinical outcomes in patients with symptomatic greater trochanteric pain syndrome. Recently the understanding of the nature of this disease has evolved. Gluteal tendinopathy is believed to be the main contributory factor rather than bursal inflammation.
Conclusion: Varying outcome measures were used to assess pain and functional outcomes with short follow ups and small sample sizes. Considering these factors, PRP seems a viable alternative treatment with the current evidence in patients, refractory to conservative measures.
Juventix Regenerative Medical is an industry leader in the regenerative medical field. Our Platelet Rich Plasma Kits are FDA cleared and designed for safety, sterility and effectiveness. Our kits are scientifically manufactured to provide a platelet concentrate, devoid of red blood cells with a minimum number of leukocytes, critical to the regenerative process.
Juventix Regenerative Medical offers a patent pending LED Activator to activate the platelets and begin the regenerative process. The activation is a critical step in the release of cytokines, growth factors and bio-active proteins from the alpha granules on the platelets and is accomplished with LED light. This negates the use of chemical additives such as calcium chloride, thrombin and collagen. This activation process by LED light provides sustained growth factor release versus older methods of activation while adhering to the minimal manipulation guideline of the FDA.
Juventix Regenerative Medical supplies a bio-incubator that transforms the Platelet Rich Plasma into an Injectable Platelet Rich Fibrin. The platelet rich Fibrin, commonly called the “second generation of platelet products” has different cytokines and growth factors than the original PRP. These different cytokines provide an anti-inflammatory environment and can be utilized confidently in inflammatory conditions.
Juventix Regenerative Medical has many products, services and devices for the regenerative medical professional and med spa owner. These products include the DermaMend LLLT, the PhysioPro shockwave, the EXD shockwave for erectile dysfunction and tissue-based products such as exosomes, offered through our collaboration with Evolutionary Biologics.
RESTORE, REVIVE, REGENERATE- JUVENTIX REGENERATIVE MEDICAL
Regenerative Regards,
Dr. Robert McGrath