Cartilage is a resilient type of connective tissue in the body.
The matrix of cartilage is composed of glycosaminoglycans, proteoglycans, collagen fibers and elastin.
Cartilage has specialized cells called chondrocytes that produce large amounts of collagenous extracellular matrix, rich in elastin fibers and proteoglycans.
Cartilage does not contain blood vessels or nerves. However, the meniscus of the knee does have a very minimal blood supply. Nutrition is supplied to the chondrocytes by diffusion.
The compression of the articular cartilage or flexion of the articular cartilage generates fluid flow which assists in the availability of nutrients to the chondrocytes. Therefore, compared to other areas in the body, cartilage has a very slow repair rate relative to other tissues possessing a significant blood supply.
Articular cartilage is dependent on the molecular composition of the extracellular matrix in the joint space. The extracellular matrix consists mainly of collagens and proteoglycans. The main proteoglycan is aggrecan which forms large aggregates with hyaluronic acid. These aggregates bind to water and hold water in the joint space. The collagen in the extracellular matrix is collagen type 2. This constrains the proteoglycans. This complex of the extracellular matrix responds to tensile and compressive forces experienced by the cartilage.
Cartilage growth is basically matrix deposition but also can refer to the growth and remodeling of the extracellular matrix.
Cartilage has vast mechanical properties and can respond to friction, compression and shearing. It has viscoelastic properties. However, cartilage has limited repair capabilities.
Chondrocytes are bound in lacunae and cannot migrate to areas of damage. Therefore, with limited blood supply and the lack of chondrocytes in a damaged area, cartilage is difficult to heal. The deposition of new matrix is extremely slow.
Cartilage repair procedures can make the advancement of osteoarthritic disease worse.
Osteoarthritis
Osteoarthritis is a disease of the entire joint, but the most affected area is the cartilage. The cartilage covering the femur is thinned and ultimately worn away exposing the bone surface to compression and friction. The meniscus becomes brittle and shearing forces cause tears.
In osteoarthritis, increased expression of inflammatory cytokines and chemokines cause aberrant changes in chondrocyte function which leads to catabolic activity. This is mediated by matrix metalloproteinases and aggrecanases.
Treatments and overall cures for osteoarthritis have been explored for many years. They have been tailored for the most part, to modify the inflammatory microenvironment in the joint space, repair the damage surgically and attempt to replace lost cartilage.
With the increase in the aging population worldwide, the incidence of osteoarthritis especially in the knee joint, has increased annually. In the population greater than 65 years old, the rate is 50% or greater. Knee osteoarthritis is now common in the middle-aged population and even in younger groups due to sports activity. The purpose and quest of the non-surgical treatment for knee osteoarthritis is the reduction of pain, to improve function and to avoid surgical intervention for as long as possible.
However, in recent years, regenerative therapies have shown good potential for the treatment of many diseases including osteoarthritis.
Regenerative Options
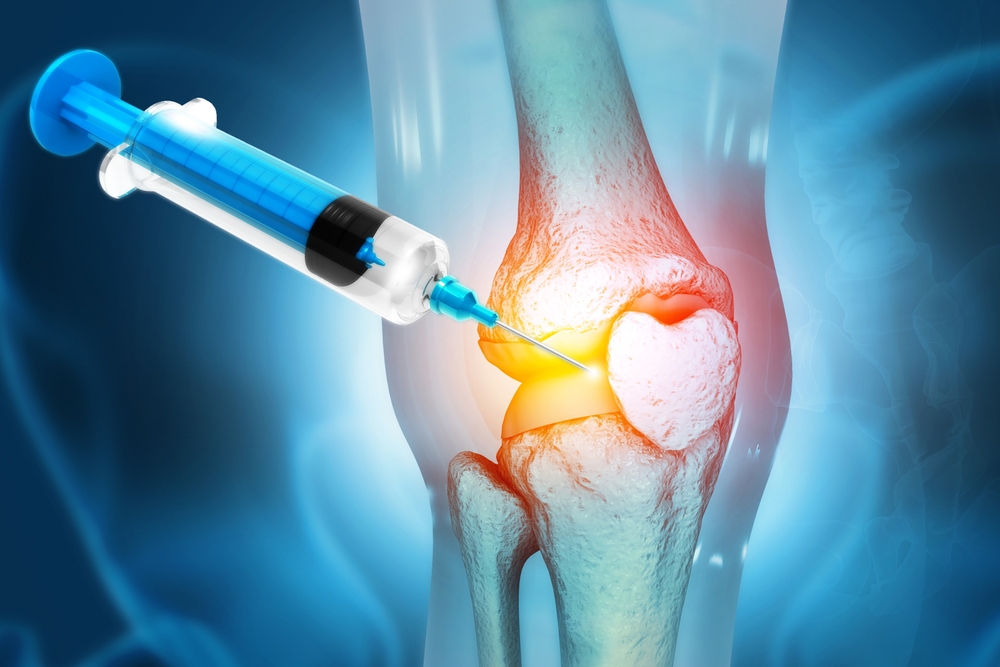
Hyaluronic acid is a nonsulfated glycoaminoglycan distributed widely throughout connective, epithelial and neuronal tissues. Hyaluronic acid is a major component of synovial fluid and increases the viscosity of the fluid. Hyaluronic acid is an important component of articular cartilage where it acts as a protective coat around each chondrocyte. With aggrecan, large aggregates form which bind water and are responsible for the cartilage resistance to compressive forces. In a 2020 meta-analysis, intra-articular injection of hyaluronic acid improved both pain and function. Hyaluronic acid has been used to supplement the loss of HA in the joint space for patients with osteoarthritis. This loss is typically greater than 50% of this substance in osteoarthritis.
Platelet Rich Plasma is an autologous blood concentrate, rich in cytokines, growth factors and bioactive proteins. These growth factors and cytokines stimulate the healing of soft tissue injuries and joint pathologies. Evidence supports the use of platelet rich plasma for a vast array of medical treatments including osteoarthritis of the knee.
Mesenchymal stem cells are multipotent stromal cells that can differentiate into a variety of cell types including Osteoblasts (bone), Chondrocytes (cartilage), Myocytes (muscle) and Adipocytes which give rise to fat cells and adipose tissue. They are present in the bone marrow and adipose tissues. In the body, these are the two areas of harvest.
The youngest and most primitive mesenchymal stem cells are obtained from the umbilical cord, namely Warton’s jelly and cord blood. Warton’s jelly provides the highest concentration of these cells. Evidence supports the use of mesenchymal stem cells for regeneration of multiple bone and connective tissue treatments.
These three regenerative treatment therapies are now being used in combination in the treatment of knee osteoarthritis.
Studies
BMJ Open 2022 Nov 16;12(11):e061008 PMID 36385022
Objectives: The purpose of this meta-analysis was to investigate the efficacy and safety of mesenchymal stem cells combined with platelet rich plasma in the treatment of knee osteoarthritis.
Conclusions: 493 cases were reviewed and concluded that treatment with mesenchymal stem cells with platelet rich plasma showed good clinical efficacy in improving pain and joint function in patients with osteoarthritis of the knee.
BMC Musculoskelet Discord 2020 Apr 11;21(1):224 PMID 32278352
Background: Studies have shown that the combination of hyaluronic acid and platelet rich plasma can repair degenerated cartilage and delay the progression of knee osteoarthritis. The purpose of this study was to explore the efficacy and safety of the intra articular injection of PRP combined with HA compared with either alone in the treatment of knee osteoarthritis.
Conclusion: 941 patients were included in this analysis. Compared with intra articular injection of PRP alone, that of PRP combined with HA can improve function scores and follow up ratings.
Arthroscopy 2021 Jul;37(7):2298-2314 PMID 33713757
Purpose: To perform a network meta-analysis to evaluate clinical efficacy and treatment related adverse events of intra articular hyaluronic acid, platelet rich plasma, mesenchymal stem cells and saline at 6 and 12 months of follow up.
Conclusions: Based on the results of current research findings during 6 months of follow up, mesenchymal stem cells relieved the pain the best and PRP was the most effective for functional improvement. In HA viscosupplementation, clinical efficacy was lower than that of the biological agents during follow up which may be related to the properties of the drug.
Note: These combinations aid in the treatment but do they regenerate cartilage which degeneration of cartilage is one of the hallmarks of osteoarthritis?
PLoS One 2024 Mar 8;19(3):e0295876 PMID 38457479
Background: Mesenchymal stem cells hold promise for osteoarthritis treatment, potentially enhanced by combining with platelet rich plasma and hyaluronic acid. This study aimed to assess the synergy of MSCs, PRP and HA and determine optimal MSC sources to treat early-stage OA.
Conclusions: ARTHROSCOPIC GUIDED APPLICATION OF PRIMARY CULTURED SYNOVIAL MSC IN POPLITEAL PLATELET RICH PLASMA MEDIA WITH HYALURONIC ACID, EFFECTIVELY REGENERATES CARTILAGE DEFECTS AND IMPROVES CLINICAL OUTCOMES IN EARLY-STAGE OSTEOARTHRITIS.
In this landmark study, bone marrow harvest resulted in poor structural quality of the repaired cartilage. The author used mesenchymal stem cells which were harvested from synovial membranes. He stated, “the potential of synovial mesenchymal stem cells can be maximized by combining with other regenerative agents including Platelet Rich Plasma and Hyaluronic Acid”.
Integrative Practice Solutions and Juventix Regenerative Medical have been involved in regenerative therapies for years. Starting with Hyaluronic Acid injections administered by fluoroscopic guidance, unloading bracing and physical therapies, IPS was in the forefront of osteoarthritis treatment. The story continued with the formation of Juventix Regenerative Medical. Regenerative therapies such as Platelet Rich Plasma and Platelet Rich Fibrin were perfected as far as cost, safety and ease of office use. Many services, devices and applications have been added over the years as the field of regenerative treatment and aesthetics is in a constant flux. Collaboration with leaders in the field on tissue biologics has been included so Juventix can offer these products to our regenerative providers.
Integrative Practice Solutions and Juventix Regenerative Medical has the knowledge and services to provide all that is currently recommended to restore cartilage as per this landmark study.
Regenerative Regards,
Dr. Robert McGrath