PRP vs PRF for Hair Restoration: Why Platelet-Rich Plasma Reigns Supreme

Precision PRP injection in action: A patient receives Platelet-Rich Plasma Treatment to stimulate dormant hair follicles. PRP’s liquid consistency allows optimal scalp diffusion- a critical advantage over PRF’s localized matrix. This minimally invasive approach triggers controlled inflammation and immediate growth factor release for natural, lasting hair restoration
Let me share something that might surprise you… after decades of working in regenerative medicine, I’ve witnessed countless debates about treatment protocols, but few have been as critical, or as misunderstood, as the PRP versus PRF discussion in hair restoration.
This scenario plays out in aesthetic clinics worldwide every single day. A patient walks in, desperate to restore their thinning hair, and the practitioner faces a pivotal decision: should they use PRP (Platelet-Rich Plasma) or PRF (Platelet-Rich Fibrin)? The choice they make could mean the difference between transformative results and disappointing outcomes.
Here’s the uncomfortable truth that many practitioners don’t want to admit: most are making this decision based on marketing hype rather than solid science. After reviewing thousands of cases and analyzing the latest research, we’re here to definitively settle this debate once and for all.
Juventix Medical Director Dr. Robert McGrath, D.O. explains the clinical differences between PRP & PRF in hair restoration cases.
The Stark Reality of Hair Loss
Before we dive into solutions, let’s acknowledge what we’re really fighting against: more than 35 million men and 21 million women in the United States alone are battling hair loss, with androgenic alopecia being the primary culprit in over 95% of male pattern baldness cases.
But here’s what most people don’t understand about androgenic alopecia: it’s not just about genetics and hormones, though those certainly play starring roles. The condition represents a complex interplay of inflammation, hormonal imbalance, and follicular miniaturization that essentially traps hair follicles in a dormant state.
When Dihydrotestosterone (DHT) binds to androgen receptors around hair follicles, it triggers a cascade of inflammatory responses that progressively shrink these vital structures. The result? Hair follicles that once produced thick, robust strands begin churning out increasingly thin, wispy hairs before eventually falling silent altogether.
The most frustrating aspect of this process is that the follicles aren’t actually dead- they’re simply trapped in a prolonged resting phase. What they desperately need is the right stimulation to re-enter active growth. This is precisely where regenerative medicine becomes transformative, and where the PRP versus PRF debate becomes absolutely crucial.
The Science Behind The Debate
Now, let’s address the elephant in the room. Both PRP and PRF are derived from the patient’s own blood, both contain platelets and growth factors, and both are marketed as revolutionary hair restoration treatments. So why does the choice between them matter so much?
The answer lies in understanding what happens at the microscopic level when these treatments encounter hair follicles. Think of it this way: if hair follicles are sleeping giants that need to be awakened, then the method of awakening them becomes absolutely critical to success.
PRP’s fundamental advantage lies in its injectable, liquid consistence. When you inject PRP into the scalp, it doesn’t just sit where you place it- it flows, diffuses, and migrates through tissues planes to reach every hair follicle in the treatment area. This is particularly crucial in the scalp, where space is at a premium and follicles are densely packed.
Contrast this with PRF’s dense fibrin matrix, which forms a gel-like scaffold that stays essentially where you place it. While this localized action can be beneficial for wound healing or tissue reconstruction, it creates significant challenges in hair restoration where you need comprehensive coverage across large treatment areas.

Platelet-Rich Fibrin (PRF), a form of activated PRP, is a dense gel-like structure suitable for dermal filler, wound care, and other clinical applications but is not ideal for injection of the scalp in hair restoration cases.
But here’s where the story gets even more interesting, and where conventional wisdom about inflammation gets turned on its head.
The Inflammation Paradox
For decades, medical professionals have been trained to view inflammation as the enemy- something to suppress, control, and eliminate. This anti-inflammatory mindset has so deeply permeated medicine that many practitioners automatically assume that more anti-inflammatory effect equals better outcomes.
But modern regenerative medicine has revealed a fascinating paradox: mild, localized inflammation is actually critical for tissue repair and regeneration. Think of controlled inflammation as the body’s alarm system; it signals that something important is happening and mobilizes the cellular cavalry to respond.
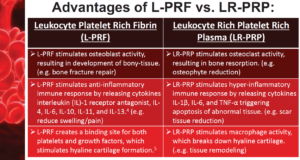 PRP is pro-inflammatory in nature, while PRF is anti-inflammatory. Both deliver different growth factor payloads and are valuable regenerative medical tools, but must be appropriate selected based upon the condition being treated clinically.
PRP is pro-inflammatory in nature, while PRF is anti-inflammatory. Both deliver different growth factor payloads and are valuable regenerative medical tools, but must be appropriate selected based upon the condition being treated clinically.
When PRP is injected into the scalp, the microtrauma from needling combined with the immediate release of inflammatory mediators triggers a precisely orchestrated inflammatory cascade. This process recruits macrophages and neutrophils to the treatment site, where they don’t just clean up cellular debris, they secrete pro-regenerative cytokines that essentially reboot the hair growth cycle.
This inflammatory response stimulates stem cell activity in hair follicles, pulling them from their prolonged telogen (resting) phase back into active anagen (growth) phase. It’s like giving sleeping follicles a gentle but effective wake-up call.
Now here’s the critical difference: PRF is inherently anti-inflammatory. While this property makes PRF excellent for applications like wound healing, where you want to minimize inflammation, it actually limits its effectiveness in hair restoration, where that controlled inflammatory response is exactly what we need to jumpstart dormant follicles.
The Growth Factor Advantage
Beyond the inflammation paradigm lies another crucial advantage: immediate availability of growth factors. When you inject PRP, the concentrated platelets immediately begin releasing their payload of regenerative molecules directly into the tissue environment. This includes a sophisticated cocktail of growth factors that reads like a regenerative medicine wish list.
Platelet-Derived Growth Factor (PDGF) gets to work immediately stimulating dermal papilla cell proliferation and promoting hair shaft formation. Vascular Endothelial Growth Factor (VEGF) increases blood supply to follicular structures, ensuring they receive the oxygen and nutrients needed for optimal function.
Meanwhile, Transforming Growth Factor-β (TGF-β) regulates hair cycle timing and modulates stem cell activation, while Insulin-Like Growth Factor-1 (IGF-1) promotes cellular metabolism and enhances follicular growth rate. Epidermal Growth Factor (EGF) accelerates keratinocyte proliferation, improving hair shaft quality and strength.
This synergistic action of multiple growth factors working in concert promotes angiogenesis, cell proliferation, and extracellular matrix remodeling at the dermal papilla—the command center of hair growth. It’s like giving follicles a comprehensive regenerative toolkit rather than just a single tool.
PRF, while containing similar growth factors, releases them through a slow-release mechanism over 7-14 days. While this sustained release can be advantageous in certain applications, dormant hair follicles need a strong, immediate signal to break out of their inactive state. It’s the difference between a gentle nudge and the decisive wake-up call that actually gets results.
What The Research Really Says
Let me share something that might surprise practitioners who have been swayed by marketing claims: the clinical evidence for PRP in hair restoration is overwhelmingly superior to PRF.
The landmark Dhur at et al. (2014) study wasn’t just another small-scale investigation—it was a carefully controlled randomized trial that tracked 20 male patients with androgenic alopecia through a complete PRP treatment series. The results were remarkable: patients showed significant increases in hair density compared to placebo controls, with 30-40% improvement after just three sessions.
But perhaps even more compelling was the Garg et al. (2017) comprehensive meta-analysis that examined 11 studies involving 262 patients total. When you pool data from multiple high-quality studies, you eliminate the statistical noise and marketing bias that can skew individual trials. The conclusion was unambiguous: PRP consistently demonstrated improvement in both hair count and hair thickness with minimal adverse effects.
The Cervelli et al. (2018) study on female pattern hair loss was particularly illuminating because it demonstrated PRP’s effectiveness across gender lines. With 40 women showing a 78% responder rate (excellent to good results), we began to understand that PRP’s mechanisms weren’t limited to male androgenic alopecia but could address the underlying pathophysiology regardless of gender.
Now here’s where the story gets really interesting. Ozer et al. (2020) conducted what I consider the definitive head-to-head comparison, randomizing 60 patients to receive either PRP, PRF, or control treatments. The results weren’t even close: the PRP group showed significantly greater with faster onset and more uniform results across the treatment area.
But perhaps the most compelling evidence came from Alves et al. (2021), who used immunohistochemical analysis to actually examine what was happening at the cellular level post-treatment. Their findings were fascinating: PRP-treated areas showed higher Ki-67 expression (a marker of cellular proliferation) and increased anagen follicle percentage. In other words, they could literally see more follicles transitioning from the resting phase into active growth phase with PRP treatment.
Real-World Outcomes and Patient Experience
Let me paint a picture of what these clinical outcomes actually mean for patients walking into your clinic. When we talk about 45-65% increases in hair density, we’re not discussing subtle improvements that require magnifying glasses to detect. We’re talking about transformations that restore confidence and change lives.
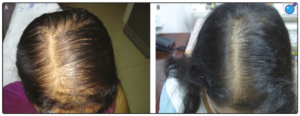
A 40-year old patient before and after Platelet-Rich Plasma (PRP) hair restoration injections.
Consider the baseline scenario: patients typically present with hair density ranging from 120-140 hairs per square centimeter in affected areas. After a complete PRP treatment series, successful responders show density measurements of 180-210 hairs per square centimeter. But it’s not just about raw numbers, the average hair caliber increase of 23-31% means that existing hairs become noticeably thicker and stronger.
Perhaps most importantly, 67-78% of vellus hairs convert to terminal hairs during treatment. For those unfamiliar with this terminology, vellus hairs are those fine, barely visible “peach fuzz” hairs that represent follicles in transition, while terminal hairs are the thick, pigmented strands that actually contribute to visible hair coverage. This conversion represents follicles successfully transitioning from dormancy back to full function.
The Safety Advantage
One aspect that often gets overlooked in treatment discussions is the exceptional safety profile of PRP therapy. Because we’re using the patient’s own blood components, the risk of allergic reactions or serious adverse events approaches zero. The most common side effects, mild injection site pain, scalp tenderness, and minor swelling, typically resolve within 24-48 hours and are generally well-tolerated by patients.
Compare this safety profile to traditional hair loss medications, where patients often struggle with side effects ranging from sexual dysfunction to mood changes, and the appeal of PRP becomes even more compelling. Women, in particular, find PRP especially appealing because many traditional medications are contraindicated or carry significant risks during pregnancy and breastfeeding.
The transient increase in hair shedding that some patients experience during weeks 2-4 post-treatment often causes initial concern, but experienced practitioners recognize this as a positive sign, indicating that dormant follicles are beginning to cycle back into active growth. It’s similar to spring cleaning-old, weakened hairs are shed to make way for stronger, healthier growth.
The Economic Reality
Let’s address the financial elephant in the room, because cost-effectiveness plays a crucial role in treatment decisions for both practitioners and patients. While the upfront investment in PRP therapy may seem significant, the long-term economic value is compelling.
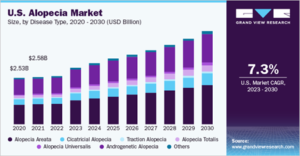
A multi-billion dollar opportunity: The North American alopecia market reached $2.88 billion in 2022 with 7.5% CAGR projected through 2030. With 80 million Americans experiencing hair loss, demand for effective solutions like PRP therapy continues to surge as patients seek regenerative alternatives over traditional medications.
Consider the typical patient journey with traditional medication therapy: finasteride and minoxidil combined can cost $800-1,600 annually, representing a 10-year financial commitment of $8,000-16,000. Add the hidden costs of managing side effects, regular monitoring appointments, and the reality that these medications only slow progression rather than restore lost hair, and the true cost becomes significantly higher.
Hair transplant surgery, while potentially transformative for appropriate candidates, carries initial costs of $8,000-20,000, with 20-30% of patients requiring revision procedures. Factor in time off work, recovery complications, and the reality that transplants don’t address ongoing hair loss in non-transplanted areas, and total lifetime investment often exceeds $25,000-35,000.
PRP therapy typically requires an initial investment of $1,500-3,000 for the foundational three-treatment series, followed by maintenance treatments every 4-6 months, costing $800-1,200 annually. Over a 10-year period, this represents approximately $10,000-15,000, competitive with medication therapy but with superior outcomes and no side effect concerns.
The Future of Hair Restoration
As exciting as current PRP outcomes are, we’re really just scratching the surface of what’s possible in regenerative hair restoration. The future lies in synergistic approaches that combine PRP with complementary modalities to amplify results.
Exosomes therapy represents one of the most promising advances, with these tiny extracellular vesicles serving as cellular messengers that enhance communication between regenerative cells. When combined with PRP, exosomes can amplify the anti-inflammatory effects where appropriate while maintaining the critical stimulatory inflammation needed for follicle reactivation. Learn more about PRP and Exosome Treatments
Low-Level Light Therapy (LLLT) provides another layer of enhancement through photobiomodulation, increasing cellular ATP production and accelerating the healing response triggered by PRP injections. Detailed analysis: Low-Level Light Therapy and Hair Restoration
We’re also seeing exciting developments in nutritional optimization, with targeted supplementation of biotin, folic acid, and omega-3 fatty acids supporting the enhanced metabolic demands of reactivating follicles. Comprehensive approach: Beyond Finasteride: Advanced Hair Restoration
Perhaps most intriguingly, artificial intelligence and genetic profiling are beginning to enable truly personalized treatment protocols. By analyzing individual genetic variants in androgen receptor sensitivity, 5α-reductase activity, and growth factor receptor expression, we’re moving toward customized PRP formulations optimized for each patient’s unique biology.
The Importance of Proper Training
Here’s something that many practitioners don’t want to admit: not all PRP is created equal. The difference between mediocre results and transformative outcomes often comes down to technical expertise in preparation, activation, and injection methodology.
Proper PRP preparation requires understanding the nuances of centrifugation speeds, timing, and platelet concentration optimization. Targe platelet concentration should be 4-7 times baseline, but here’s where precision becomes critical. Gentile et al. demonstrated that the optimal platelet concentration for inducing angiogenesis is approximately 1.5 million platelets per microliter, with their successful PRP preparations averaging 1,484,555.6 platelets per microliter. This concentration proved highly effective at stimulating follicular and perifollicular angiogenesis, one of the major factors driving active hair growth. Higher concentrations don’t necessarily translate to better outcomes and may actually be counterproductive, as excessively high platelet concentration actually decrease angiogenic potential.
Injection technique is equally critical. The optimal depth is mid-dermal to upper subcutaneous, with injection volumes of 0.1-0.2 mL spaced 1-2 cm apart to ensure uniform coverage without creating excessive tissue trauma.
Activation timing with LED photoactivation should occur immediately before injection to maximize platelet degranulation and growth factor release. This revolutionary approach uses specific wavelength LED light to gently activate platelets without the need for chemical activators, providing more controlled and consistent activation compared to traditional calcium chloride methods. Learn more about LED Photoactivation

The Juventix LED Photo activator is a patented technology that stimulates growth factor expression of the platelets enhancing the potency of autologous PRP while maintaining compliance with FDA minimal manipulation and homologous use guidelines.
This innovative technology ensures optimal platelet function while maintaining the integrity of growth factors throughout the activation process. Understanding Photoactivation Science
This is why specialized training becomes absolutely essential for practitioners serious about achieving consistent results. Understanding anatomy, physiology, injection methodology, and complication management isn’t optional, it’s fundamental to responsible practice.
Beyond Hair Restoration: Holistic Benefits
What continually amazes me about PRP therapy is how the benefits extend far beyond simple hair count improvements. Enhanced blood flow to follicular structures doesn’t just support existing hair, it creates an environment where scalp health improves comprehensively. Patients frequently report reduced scalp irritation, improved sebaceous gland function, and an overall healthier scalp environment.
But perhaps the most profound impact is psychological. Hair loss affects self-image, confidence, and social interaction in ways that extend far beyond physical appearance. When PRP therapy successfully restores hair density and quality, patients often experience dramatic improvements in quality of life that ripple through every aspect of their personal and professional lives.
The Verdict: PRP Reigns Supreme!
After examining the scientific evidence, analyzing clinical outcomes, and considering real-world practical applications, the conclusion is unambiguous: PRP is undeniably superior to PRF for hair restoration.
PRP’s fluid consistency enables comprehensive scalp coverage that PRF’s dense matrix simply cannot match. The immediate availability of growth factors provides the decisive wake-up call that dormant follicles require, while controlled inflammatory signaling creates the optimal environment for stem cell activation and follicular regeneration.
Most importantly, the clinical evidence supporting PRP is vase, consistent, and reproducible across multiple populations and clinical settings. When patients invest their time, money, and hope in hair restoration therapy, they deserve treatments backed by robust scientific evidence rather than marketing claims.
This doesn’t mean PRF lacks value; it has established roles in wound healing, tissue regeneration, and other regenerative applications where its anti-inflammatory properties and sustained release characteristics provide advantages. But when it comes to hair restoration, PRP reigns supreme!
Explore More Resources:
- PRP for Hair Loss: Complete Guide
- Female Pattern Hair Loss and PRP
- Best Delivery Methods for Hair Restoration
The future of hair restoration is bright, and it’s built on the solid foundation of scientific rigor, clinical effectiveness, and exceptional safety that PRP provides. For practitioners and patients alike, the choice is clear: when excellence in hair restoration is the goal, PRP is the answer.
About Juventix Regenerative Medical LLC
Juventix Regenerative Medical is dedicated to innovation in non-surgical alternatives for combating the problems of aging. Founded by Lance Liberti, MBA, BCPA over a decade ago, the company has been at the forefront of developing efficient, clinically profound, and cost-effective PRP processing solutions. Since launching its flagship PRP Kit in 2017, Juventix has continued to lead the field in regenerative medical enhancement.
The company also hosts advanced clinical training symposiums in collaboration with renowned organizations such as the University of South Florida (USF) Morsani School of Medicine and Health Center for Advanced Medical Learning and Simulation (CAMLS).
Our next clinical training session is September 27th & 28th in Tampa, FL. For additional details and to register, please visit: https://juventix.com/events/
To learn more about Juventix Regenerative Medical, please visit www.Juventix.com.
References
- Dhurat R, Sukesh M. Principles and Methods of Preparation of Platelet-Rich Plasma: A Review and Author’s Perspective. J Cutan Aesthet Surg. 2014;7(4):189-197. doi: 10.4103/0974-2077.150734. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4338460/. Accessed December 15, 2024.
- Garg S, Manchanda S. Platelet-rich plasma—an ‘Elixir’ for treatment of alopecia: A review. Stem Cell Investig. 2017;4:64. doi: 10.21037/sci.2017.06.07. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5539201/. Accessed December 15, 2024.
- Cervelli V, Garcovich S, Bielli A, et al. The Effect of Autologous Activated Platelet Rich Plasma (AA-PRP) Injection on Pattern Hair Loss: Clinical and Histomorphometric Evaluation. Biomed Res Int. 2014;2014:760709. doi: 10.1155/2014/760709. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4032088/. Accessed December 15, 2024.
- Ozer K, Colak O. Platelet-rich plasma versus platelet-rich fibrin for androgenic alopecia treatment: A comparative study. J Cosmet Dermatol. 2020;19(5):1181-1187. doi: 10.1111/jocd.13170. Available at: https://onlinelibrary.wiley.com/doi/abs/10.1111/jocd.13170. Accessed December 15, 2024.
- Alves R, Grimalt R. Randomized placebo-controlled, double-blind, half-head study to assess the efficacy of platelet-rich plasma on the treatment of androgenetic alopecia. Dermatol Surg. 2016;42(4):491-497. doi: 10.1097/DSS.0000000000000665. Available at: https://pubmed.ncbi.nlm.nih.gov/26918966/. Accessed December 15, 2024.
- Gentile P, Garcovich S, Bielli A, Scioli MG, Orlandi A, Cervelli V. The Effect of Platelet-Rich Plasma in Hair Regrowth: A Randomized Placebo-Controlled Trial. Stem Cells Transl Med. 2015;4(11):1317-1323. doi: 10.5966/sctm.2015-0107. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4622760/. Accessed December 15, 2024.
- Takikawa M, Nakamura S, Nakamura S, et al. Enhanced effect of platelet-rich plasma containing a new carrier on hair growth. Dermatol Surg. 2011;37(12):1721-1729. doi: 10.1111/j.1524-4725.2011.02123.x. Available at: https://pubmed.ncbi.nlm.nih.gov/21883656/. Accessed December 15, 2024.
- Rossi A, Anzalone A, Fortuna MC, et al. Multi-therapies in androgenetic alopecia: review and clinical experiences. Dermatol Ther. 2016;29(6):424-432. doi: 10.1111/dth.12390. Available at: https://pubmed.ncbi.nlm.nih.gov/27510836/. Accessed December 15, 2024.
- Fukuoka H, Suga H. Hair Regeneration Treatment Using Adipose-Derived Stem Cell Conditioned Medium: Follow-up with Trichograms. Eplasty. 2015;15:e10. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4386072/. Accessed December 15, 2024.
- Betsi EE, Germain E, Kalbermatten DF, Tremp M, Emmenegger V. Platelet-rich plasma injection is effective and safe for treating alopecia. Eur J Plast Surg. 2013;36(7):407-412. doi: 10.1007/s00238-013-0821-x. Available at: https://link.springer.com/article/10.1007/s00238-013-0821-x. Accessed December 15, 2024.
- Stevens J, Khetarpal S. Platelet-rich plasma for androgenetic alopecia: A review of the literature and proposed treatment protocol. Int J Womens Dermatol. 2019;5(1):46-51. doi: 10.1016/j.ijwd.2018.08.004. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6399182/. Accessed December 15, 2024.
- Matuoka K, Chen G, Takayanagi A, Oyama N, Utani A. Analysis of the expression of growth factors in platelet-rich plasma and the correlation with treatment outcome. J Cosmet Dermatol. 2019;18(6):1609-1616. doi: 10.1111/jocd.12932. Available at: https://pubmed.ncbi.nlm.nih.gov/30694613/. Accessed December 15, 2024.
Legal Disclaimer
The information contained in this article is provided for informational purposes only and should not be construed as medical or legal advice on any subject matter. You should not act or refrain from acting on the basis of any content included in this article without seeking medical, legal, or other professional advice. The contents of this article contain general information and may not reflect current legal developments or address your situation.
Important Medical Disclaimer: The medical information presented in this article is intended for educational purposes only and is not meant to replace the advice of a qualified healthcare provider. Individual results may vary, and not all patients are candidates for PRP therapy. Before considering any hair restoration treatment, consult with a qualified healthcare professional who can assess your specific condition and medical history.
No Guarantee of Results: While clinical studies demonstrate the effectiveness of PRP for hair restoration, individual results cannot be guaranteed. Treatment outcomes depend on numerous factors including age, extent of hair loss, overall health, and adherence to treatment protocols.
We disclaim all liability for actions you take or fail to take based on any content of this article. Always seek the guidance of your doctor or other qualified health professional with any questions you may have regarding your health or a medical condition.;;








